Blog Posts
Swim Safety
It’s that time again! Time for spring break, family vacations, and before you know it… Summer!!!
When we think of swim and water safety for our little ones we usually think about supervision, life vests, floats and lifeguards. All of these are important, but so is your child’s swimsuit. We aren’t talking about SPF50 swimwear (which we are totally a fan of) but rather the color the swimsuit your child wears. It can mean the difference between life or death, especially in a public pool situation, at the beach, or at the lake.
We found these handy color charts from Alive-Solutions to help illustrate how important it is for your child to have a bright colored swim suit! (We are not affiliated with Alive-Solutions). The pictures show how a swimsuit is seen under water at different depths.

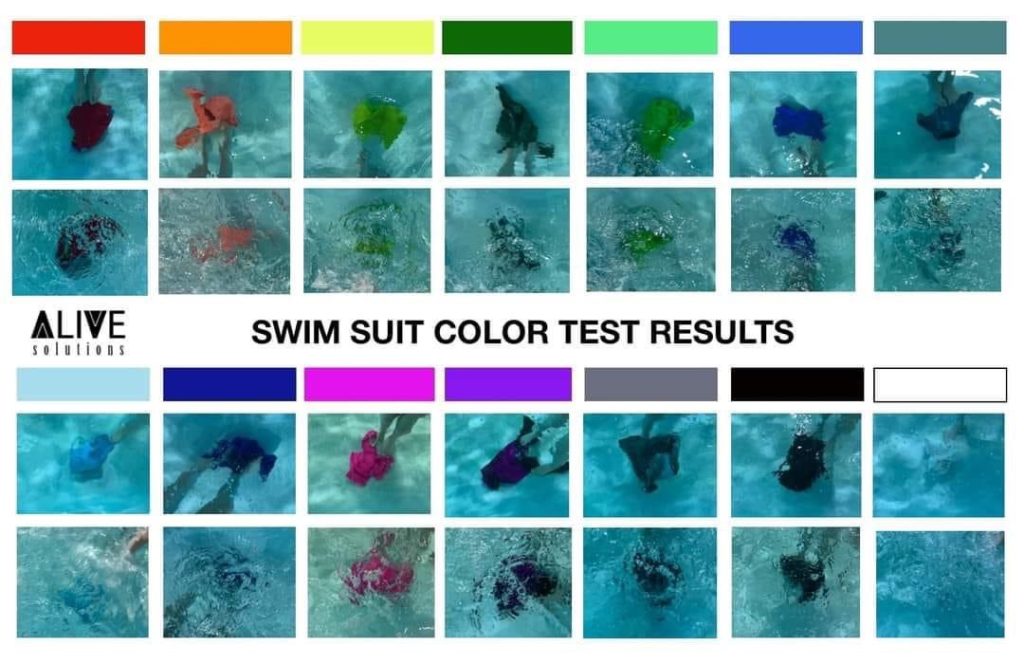

So when thinking of picking out that cute swimsuit for your child this year, keep this chart in mind and pick a bright color that will make it easier for you to see!
Xoxo
Ell & Ali
Breastfeeding

BREASTFEEDING TIPS & TRICKS
Trying to prepare yourself for breastfeeding?
Feeling overwhelmed with breastfeeding?
Trying to troubleshoot your current breastfeeding issues?
You’re in the right place!
*Disclaimer: We always recommend speaking with your Doctor, OBGYN, Midwife, and/or Lactation Consultant for any issues or concerns that you have. This is not meant to be taken as medical advice.*
Hey! It’s Ell here! Ali and I wanted to share with you some of the tips and tricks that we have learned from our doctors, lactation consultants, and through experience. Ali has been breastfeeding her daughter for a year and a half, and I have been breastfeeding my son for a year. If you are experiencing issues with breastfeeding, have questions or concerns, we recommend that you contact a certified lactation consultant (LC), your midwife or pediatrician. As much as our tips and tricks are here to help, they do not replace the valuable input of a certified LC that can watch what you are doing and help you make hands on adjustments. Most insurances cover LC appointments. In addition, both of us highly recommend that if you do not have people around you that are well versed in breastfeeding, that you consider taking a breastfeeding class. Most hospitals have free breastfeeding classes that you can take prior to giving birth. Ali wanted me to share that if she had not taken the breastfeeding class, she probably would have given up on breastfeeding early on. Like me, Ali didn’t have anyone around her that had recently breastfed, she knew nothing about the challenges that might occur, how and when to use breast shields, ways to hold the baby for breastfeeding, or what cluster feeding was. All of this she was able to learn in her breastfeeding class. When we both ran into issues during our breastfeeding journey, we turned to certified LCs.
Also, before we go on, we would like to say FED IS BEST!!!! You are one amazing mother no matter if you breastfeed your baby, bottle feed formula, or do a combination of both!
The first thing I always hear from LCs and Doctors is how natural breastfeeding is. They make it sound easy and like your body just knows how to do it. I am going to start out by saying, it takes work and trial and error (just like with bottle feeding formula). It takes perseverance and an adjustment period for you and your baby to learn how to feed together. This is normal! Very few women breastfeed without at least one or two issues arising.
Tips & Tricks for Breastfeeding
- Have realistic expectations and give yourself grace. Every person’s body is different.
- HYDRATE! HYDRATE! HYDRATE! Hydration is the key to breastfeeding. In order to get your breast milk production to its optimal level, stay hydrated. Water or water with electrolytes is best. Stay away from diuretics as much as possible. I personally utilize a mix of water, carbonated water, and electrolyte drinks with no sugar added.
- FACE SYMMETRY of the baby to the breast is most important for pain free feeding and a good latch. Try to make sure that you baby’s chin, cheeks, and nose touch the breast equally. The nose should not be smashed into the breast but should rather gently touch its tip to the breast. If you notice that your child has one portion of their face more on the breast, such as one cheek is touching the breast fully while the other isn’t even touching, adjust your baby’s head to have it touching evenly. It sometimes will help to unlatch your baby and relatch.
- THE HOW TOs: It is recommended by LCs that you feed your baby to their fill on one breast, let the baby rest and digest, and then switch to the other breast until they are satisfied. This is a good rule of thumb for starting, but not all babies will do this and that is okay. Remember to switch the breast you start with at each feeding. If you only feed off one breast, one breast will regularly produce more milk than the other and you will have uneven breasts. It is also normal for a baby to prefer one breast over another. Try to still have them latch and feed on both breasts.
- PAIN: If you are feeling pain, after checking your baby’s face symmetry, check your baby’s lips. Are they curled in? If they are curled in, gently try to move your baby’s lips so that they are uncurled. Relatch your baby if needed.
- BREASTFEEDING POSITIONS. Try different positions with your baby until you find what works best for the both of you. No one position is better than the other. Often times, you will find that you like a few positions and change between them as needed. In the hospital I used the football (or rugby ball) hold with my son but I’m large chested and felt like I was smothering him, so I quickly switched to the cross cradle. After going to my LC we switched to the laid back hold and to the Koala. This helped my son control my flow better and decreased his choking and sputtering. Now I’m lucky if my child doesn’t do acrobatics while he feeds lol! I will refer you to this great explanation by Medela for different positions. (I am not affiliated with Medela nor do I get paid for mentioning them.)
- CLOGGED DUCTS: Both Ali and I both ran into this issue. Feel your breasts regularly. Do you notice a hard lump? Painful when you put pressure on and around it? This is most likely a clogged duct. (We recommend seeing a doctor if you aren’t sure. Lumps in the breast can be a more serious problem that only a doctor/OBGYN can diagnose). If you have a clogged duct try: warm compresses, vibration, hot water, Epson salt in a haakaa, latch your baby as often as possible, pump if needed. Warm compresses and hot water: you can use heating pads or stand under hot water. The water should only be as hot as you can comfortably stand. There is risk of being burned if the water is too hot for you. Please be cautious. Add heat to the area often. Epson Salt Haakaa (or manual pump that similar): You can put 1tbsp of Epson salt in your Haakaa and fill with very warm water (only as hot as you can comfortably withstand). Tip the Haakaa upside down and suction it to your breast. Leave on for 10-15 minutes and repeat as necessary throughout the day. Add Vibration: They make these handy little vibrators with or without heat for breastfeeding. You can use one of these in a downward motion toward the nipple. If it is sensitive to go over the lump, start at the furthest part of the lump closest to the nipple. Repeat downward motions for 5-10 minutes. If you don’t have one of the breastfeeding vibrators, use your imagination. I’ve had a friend use an electric toothbrush and it worked! Use a combination or all of these to help get your duct unclogged. Usually, your duct will unclog within 24 hours. However, if it does not, we recommend seeking a doctor or OBGYN’s help.
- MASTITIS: This is an infection and inflammation of breast tissue. It can cause pain, swelling, warmth, redness, and fever. If you suspect you have Mastitis, see your doctor right away as antibiotics may be necessary for treatment. Left untreated, Mastitis can become a serious health issue. Ali had personal experience dealing with Mastitis and she highly recommends that breastfeeding women should check their breasts all the time as preventative maintenance because it can go sideways fast. Check all around and underneath each breast for redness and tenderness. Watch for body aches and fever.
- IS BABY GETTING ENOUGH?: Remember, a baby is always able to more efficiently get milk out of your breast than a pump. So just because your pump doesn’t show you getting a lot, doesn’t mean your baby isn’t getting more. If you are concerned about your baby’s intake please consult with your pediatrician. A good rule of thumb after the first week of birth is that your baby is having regular wet diapers (6 or more per day). For the first week of life, it is different. For the first few days it is normally two wet diapers or more, and starts to increase.
- SUPPLY: Unfortunately, as a breastfeeding mother you will most likely at some point fret and worry over your supply. Supply does not regulate until the first 4-6 weeks of breastfeeding. During this time, it is normal to have sore breasts and for them to feel rather hard. If you are an oversupplier and your baby is having trouble with the intake, try to manually express your breasts just a short amount or use your haakaa for a short time prior to feeding your baby. Be careful not to express more than needed because you can increase your supply by doing this. If you are worried about your supply and need to try to increase it, you can pump right after you feed your baby. This will allow your body enough time to recover for the next feeding. It is also helpful to note that your body produces more milk in the morning than it does in the evening. This fluctuation throughout the day is normal.
- PUMPING: Pumping is a whole other ball game. Please be sure to check with your specific pump for their directions for the settings. It is important to know that not all pumps are created equal. Each pump you use may give you a different result with output. For instance, I have used three different pumps. I have used Medela’s manual pump (and to this day it gets out the MOST milk of every pump), Spectra’s S1 that pugs into a wall, and the Willow Go portable wireless pump. Each one gets out a different amount for me. I personally went to my LC to get her to show me how to use my pump. As a rule of thumb, I pump whenever my baby ate while I was at work. This way I had enough milk for him. Prior to going to work I built up a stash in the freezer by using my haakaa on the opposite breast that my child was nursing on because of my oversupply. In addition, my LC recommended to pump after my son’s morning feeding.
- YOUR PERIOD: When your period comes back, it WILL affect your supply. Usually just prior to your period your hormones will change and your supply will slightly drop. This usually occurs for a few days and then will go back to normal toward the end of your period or after you finish your period.
- WEANING: If you find that your breastfeeding journey is coming to an end, be sure to slowly decrease how often you breastfeed. Stopping breastfeeding too abruptly can cause clogged ducts and mastitis.
- BREASTMILK STORAGE: Please refer to the CDC’s guide for proper storage and preparation of breastmilk. We would also like to add that your child’s breastfeeding needs will change as they grow. A child may feed in a cluster at night to prepare for longer sleep or may feed for frequently to accommodate for a growth spurt, before breastfeeding decreases to a normal level again. Introducing solids may also alter the amount and frequency of breastfeeding. This is all normal.
Again, the information here is just our experiences and is not intended to replace information from a medical doctor or certified lactation consultant. If you have any questions or concerns, please reach out to your Doctor, OBGYN, Midwife, or Lactation Consultant.
xoxo
Ell
